Worldwide, approximately 16 million people inject illicit substances, and three million of them have HIV infection. The use of these agents may also lead to viral hepatitis. Of the 2.5 million people who acquired HIV in 2011, a tenth of these infections were the result of injecting drug use. In some regions of Eastern Europe and Central Asia, more than four-fifths of all HIV cases originated from that practice [1, 2].

Injecting Drug Use and HIV
Injecting drug use is a global public health problem as it is responsible for many cases of human immunodeficiency virus (HIV).
Comprehensive Care Package
The World Health Organization recommends a comprehensive care package for the situation [2]. First, it supports needle and drug programs so that those who inject substances will not share syringes. In other words, drug users will have clean needles and syringes, and this lessens the risk of HIV transmission.
Second, these clients need to undergo medical treatment for their addiction, and substitution with an opioid agent, such as methadone, for the illicit chemical may make it easier to manage the dependence. Screening and counseling for HIV are essential. Moreover, clinical management and health education are necessary.
Distribution of condoms has a vital role in disease prevention, and adequate treatment of sexually transmitted infections is a requirement to lessen their spread. Moreover, since substance users are at risk for tuberculosis and viral hepatitis, clinical management of those infectious diseases is important [2].
Some have suggested the implementation of needle and syringe programs and availability of condoms in prisons. Though many correctional facilities object to these approaches, there have been trials of them in various parts of the globe.
Clinical Research Trials
Clinical research suggests that it is possible to lower the susceptibility of injecting drug users to HIV through pre-exposure prophylaxis with antiretroviral medication [1]. Trials took place from 2005 to 2010 in Bangkok, Thailand. The subjects came from 17 substance abuse and dependence treatment centers there, and 2,413 of them entered the study as volunteers.
These participants were between the ages of 20 and 60, and all of them were HIV seronegative when they joined the trial. They received HIV testing and counseling. The investigators offered methadone treatment and condoms to all of the respondents. Approximately one-half of the subjects took placebo, and the others received oral tenofovir therapy [1].
The researchers consider tenofovir a suitable antiretroviral medication for these clients as it does not interfere with the pharmacokinetics of methadone, which serves as opioid substitution therapy [1].
The scientists concluded that oral tenofovir was beneficial for reduction of HIV acquisition in injecting drug users. In other words, this antiretroviral agent may prevent an HIV-negative drug user from occurrence of the disease despite his or her exposure to the virus through shared needles and syringes [1].
References
- Choopanya, K., Martin, M., Suntharasamai, P., et al. for the Bangkok Tenofovir Study Group. (2013). Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (The Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. The Lancet, 381, 2083-2090.
2. World Health Organization. (2013). Injecting drug use. Retrieved June 20, 2013.
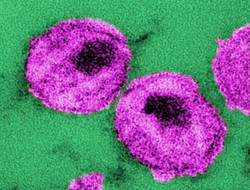
3. The photograph is a thin-section transmission electron micrograph of several human immunodeficiency virus particles. Reprinted with permission from Centers for Disease Control/Dr. A. Harrison/Dr. P. Feorino.
Conclusion
Injection drug use is one of several ways that HIV spreads across the globe, and attention to all methods of transmission will be necessary to end the pandemic.
Disclaimer
The information contained in this article is for educational purposes only and should not be used for diagnosis or to guide treatment without the opinion of a health professional. Any reader who is concerned about his or her health should contact their physician for advice.
You might also like
How to React to and Help a Loved One with CancerDealing with cancer? Learn how to react, treat and care for a loved one when ...
Do You Have Your Own Cure For Cancer?Is it possible you might be completely unaware of the cancer cure, a natural ...


 The Reality of Aspirinon 05/24/2021
The Reality of Aspirinon 05/24/2021
 An Old Microbeon 03/31/2021
An Old Microbeon 03/31/2021
 Coronavirus and Mental Illnesson 02/14/2021
Coronavirus and Mental Illnesson 02/14/2021
 Acute Ischemic Strokeon 12/25/2020
Acute Ischemic Strokeon 12/25/2020

Comments