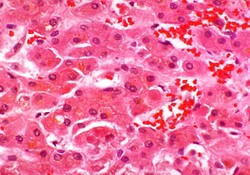
The evaluation and diagnosis of alcoholic hepatitis, as with any other medical condition, require careful history and physical examination. Laboratory assays will, of course, aid in its confirmation. Nevertheless, there may be uncertainty because the clinical and laboratory findings overlap with other diseases [1, 2].
This consideration, and others, lead to recommendation for the use of liver biopsy in these clients. Specifically, the most accurate way to confirm the presence of alcoholic hepatitis is histologic view of liver tissue. When the clinical presentation strongly suggests severity of this condition and there are plans for medical therapy, the use of liver biopsy is, in essence, a necessity [1, 2].



 The Reality of Aspirinon 05/24/2021
The Reality of Aspirinon 05/24/2021
 An Old Microbeon 03/31/2021
An Old Microbeon 03/31/2021
 Coronavirus and Mental Illnesson 02/14/2021
Coronavirus and Mental Illnesson 02/14/2021
 Acute Ischemic Strokeon 12/25/2020
Acute Ischemic Strokeon 12/25/2020

Comments