If you maintain a very clean house, you probably use a product that boasts of its antibacterial features – killing germs, bacteria and making your home safe and secure against anything that might make you or your loved ones ill. But, that same dedication to your health and those around you could also pose a grave danger.
A 2014 report by the World Health Organization (WHO), the first ever by the organization to look at antibiotic resistance, calls antibacterial resistance a serious and present danger that is impacting people of all ages and in all countries around the world.

The Dangers Of Antibiotic Resistance
Resistance to antibiotics has become a global problem and a health threat that is growing. Here's what you need to know.
What Is Antibiotic Resistance?
The problem with antibiotics is that the bacteria it is meant to eradicate grow resistant to it over time. That, in turn, means that far beyond mere household cleanliness issues, bacteria become resistant in places where you really need them to work such as in hospitals and when people are really ill. WHO even calls the problem “a major threat to public health.” The future is not looking good, the report says, and the world can look forward to a time in the near future when once treatable diseases “can once again kill.”
One of the wonders of modern medicine, antibiotics have helped people live longer, healthier and more enjoyable lives. But, the old adage about too much of a good thing is certainly becoming the case when it comes to antibiotics. WHO is calling for “significant actions to improve efforts to prevent infections and also change how we produce, prescribe and use antibiotics.”
Experts have noted that diseases and infections like MRSA, tuberculosis, diarrhea, pneumonia, urinary tract infections and gonorrhea have already been found resistant to antibiotics that are commonly used to treat the diseases.
The U.S. Centers for Disease Control and Prevention (CDC) says that each year at least 2 million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die each year as a direct result of these infections. In addition, almost 250,000 people each year require hospital care for Clostridium difficile (C. difficile) infections. In most of these infections, the use of antibiotics was a major contributing factor leading to the illness. At least 14,000 people die each year in the United States alone from C. difficile infections and many of these infections could have been prevented.
There is also an economic cost to the problem. The CDC reports that the total economic cost of antibiotic resistance to the U .S. economy ranges as high as $20 billion in excess direct healthcare costs, with additional costs to society for lost productivity as high as $35 billion a year (2008 dollars).
What Happens When Resistance Is Compromised?
Antibacterial resistance exhibits itself in several ways. If you have an infection you may find it harder to fight it off. Complications from your ailment may arise and you could more easily pass on your infection to others.
And is science going to come to the rescue? Many people are hoping so, but experts say that may not happen any time soon. The ‘pipeline’ for new antibiotics is drying up and even if new antibiotics are found, they too will eventually result in bacteria gaining resistance to them as well.
How Did This Happen?
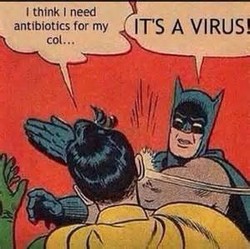
The roots of this problem came through good intentions, with a lot of help from business’ who marketed the wonders of antibacterial agents in every conceivable product. Some of the causes include using antibiotics when they were not needed – such as fighting a virus, for which antibiotics don’t work. Conversely, not taking antibiotics as prescribed created the problem as well because that failure allowed bacteria that would have otherwise been knocked out to survive and infect again. The common and widespread use of antibiotics in veterinary medicine and agriculture also helped cause the problem, experts say, because that widespread use helped build bacterial resistance even faster. Resistant bacteria can be transmitted to humans through the foods we eat.
The problem has even been made worse due to global travel. This means that the problem that may have been contained in one country can more easily spread to other countries and people when they travel abroad.
What Can You Do?
The problem is a global one, but it is one that requires everyone to take precautions. Here are some tips:
- Take precautions when traveling (such as proper vaccinations). That means not only avoiding contact with people who may be ill when away from home, but also re-considering your own travel plans if you are sick.
- Practice good hygiene. Be vigilant about washing your hands after contact with an ill family member, for example, or after being in contact with dirty surfaces or products (like raw chicken).
- Understand when and when not to use antibiotics. Viruses cause a cold or flu and antibacterial agents will have no affect. When it is prescribed, take it as ordered and don’t fail to take it until your doctor says its ok, even if you think you feel better.
- Don’t use antibiotics that have an expired date.
- Avoid using common cleaners, soaps and other household items that brag about having antibacterial agents. A good soap and hot water scrubbing will do just fine to clean your countertops.
In the U.S. the CDC has proposed a Detect and Protect Against Antibiotic Resistance Initiative (known as the AR Initiative) as part of a broader CDC strategy to target investment aimed at AR. If Congress authorizes the $30 million dollars in 2015 that has been requested the initiative would achieve a 50 percent reduction in healthcare-associated C. difficile, which saves 20,000 lives, prevents 150,000 hospitalizations, and cuts more than $2 billion in healthcare costs; a 50 percent reduction in healthcare-associated CRE infections; 30 percent reduction in healthcare-associated multidrug-resistant (MDR) Pseudomonas, a common cause of healthcare-associated infections; a 30 percent reduction in invasive MRSA; and a 25 percent reduction in MDR Salmonella infections.
A national ‘Get Smart’ educational campaign has also been launched to help people understand when antibiotics work and when they don’t; what the impact is on farms; and how proper hygiene can save lives.
You might also like
Fitness Apps – Are They Helpful?Fitness apps and games are a multi-billion dollar industry, but will they wor...
Online Pharmacies – Buyer Beware or Great Deal?Online pharmacies may be a less expensive alternative but are they safe? Shou...












 The Problem With Wizzley and Amazon Associateson 10/17/2014
The Problem With Wizzley and Amazon Associateson 10/17/2014
 Happy Wife, Happy Life: Is It True?on 10/02/2014
Happy Wife, Happy Life: Is It True?on 10/02/2014
 Arborsculpture Designs Are Beautiful And Practicalon 09/30/2014
Arborsculpture Designs Are Beautiful And Practicalon 09/30/2014
 The Religious And Immoral Actson 09/23/2014
The Religious And Immoral Actson 09/23/2014



Comments
Revisiting your wizzley brought to mind something that I meant to ask after my first reading and my first shared reactions.
Which soap would you consider the most effective as a countertop cleaner in conjunction with hot water?
TheWritingCowboy, How do alternative and homeopathic medicines approach treatment resistance?
TheWritingCowboy, It's a sobering scenario to realize that "Resistant bacteria can be transmitted to humans through the foods we eat."
I am so glad that you have written about thus. I have been banging on about this subject for years. Bacteria are, in evolutionary terms, and humans need to be more responsible.